The findings also highlight the importance of normalising weight before attempting to conceive, according to one expert.
Keeping an eye on the scales during pregnancy is important – even in women who’ve previously undergone bariatric surgery to help manage their weight.
Women with a history of bariatric surgery have a lower risk of gestational diabetes, preeclampsia and requiring a caesarean during pregnancy, but have an increased risk of delivering prematurely and having small-for-gestational age babies.
Gaining weight during pregnancy, regardless of whether a woman has had surgery, is also associated with these outcomes, yet little is known about how bariatric surgery affects postoperative pregnancy weight gain.
Now, a recent population-based cohort study from Sweden, published in JAMA Network Open, reports women with a history of bariatric surgery gain less weight during pregnancy – with pregnancy weight gain being lowest in women who fall pregnant within a year of surgery.
“There are problems with gaining too little or too much weight during pregnancy, so it’s a real balancing act,” said obstetrician, Associate Professor Alex Polyakov, from Royal Women’s Hospital.
“But the finding that women who got pregnant after bariatric surgery gained less weight is a positive one, as overweight and obese women face a lot of challenges during their pregnancy.”
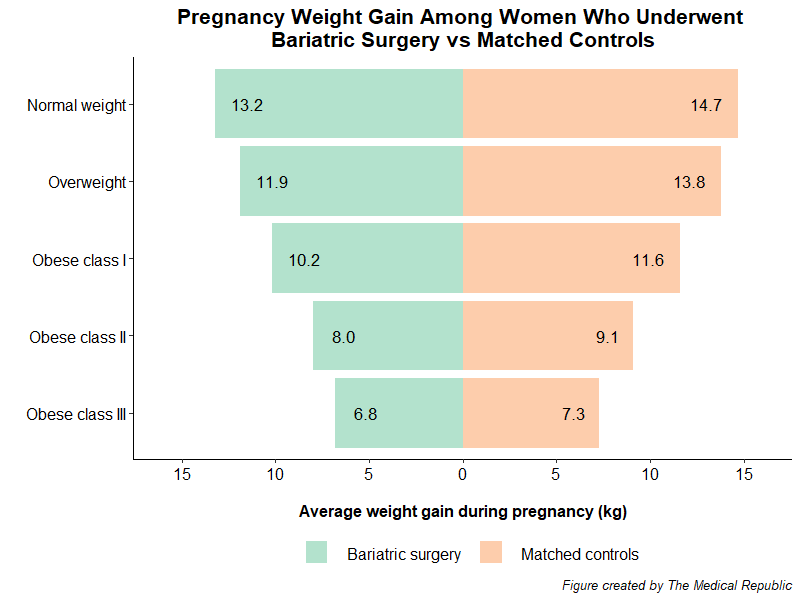
Researchers compared weight gain during pregnancy in 6300 women with a history of bariatric surgery with an equal number of women who had not had bariatric surgery.
The two cohorts were matched on factors such as age, BMI, smoking status, pre-pregnancy diabetes and hypertension. Forty percent of women in each cohort were overweight at the start of their pregnancy (BMI range: 25.0-29.9).
Women with a history of bariatric surgery gained less weight over the course of their pregnancy than their non-operated counterparts. The difference between cohorts was greatest in women of a normal weight.
Professor Polyakov questioned whether the difference of a few kilograms here and there between the two groups was clinically significant but felt the women who previously undergone surgery had still gained an appropriate amount of weight (according to international recommendations).
There was no difference in pregnancy weight gain between women who underwent a sleeve gastrectomy compared to those who had a gastric bypass.
The greatest number of babies who were small for gestational age were born to women who gained the lowest amount of weight during their pregnancy. Large for gestational age babies and acute caesarean deliveries were more common in women who gained more weight during pregnancy.
The researchers suggested the association between bariatric surgery and reduced pregnancy weight gain can be explained by the “physiological effects of altered anatomy and gut hormones” which reduced appetite and food intake.
They also noted that women who had bariatric surgery were recommended to minimise weight gain during pregnancy as a means of keeping the weight off after the procedure.
“Clinical attention to women with a history of bariatric surgery and a normal weight status in early pregnancy might be warranted,” the researchers concluded.
Professor Polyakov agreed with the researcher’s conclusion, suggesting women with a history of bariatric surgery should seek professional guidance regarding their diet and the appropriate amount of weight to gain during their pregnancy, noting women who were still obese after bariatric surgery should aim to gain a smaller amount compared to women with a normal BMI.


